
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use GLYDO (lidocaine HCl jelly) 2% safely and effectively. See full prescribing information for GLYDO (lidocaine HCI jelly) 2%.
GLYDO (lidocaine hydrochloride) 2% jelly Initial U.S. Approval: 1953
——- INDICATIONS AND USAGE ——-
GLYDO (lidocaine HCl jelly) 2% contains lidocaine, an amide local anesthetic, and is indicated in adult patients:
- for prevention and control of pain in procedures involving the male and female urethra (1}
- for topical treatment of painful urethritis (1)
- as an anesthetic lubricant for oral and nasal endotracheal intubation (1)
—– DOSAGE AND ADMINISTRATION —–
- The toxic effects of local anesthetics are additive. When using this product concomitantly with other lidocaine-containing products, consider the total dose of lidocaine and monitor patients for cardiovascular and respiratory vital signs. (2.1)
- For surface anesthesia of male adult urethra: 15 mL (300 mg lidocaine HCl) followed by additional 15 mL if needed (2.2)
- For surface anesthesia of female adult urethra: 3 mL to 5 mL (60 mg to 100 mg lidocaine HCl) (2.3)
- For lubrication for endotracheal intubation:
sufficient amount to coat the external surface of endotracheal tube (2.4) - For pediatric patients: Not more than 4.5mg/kg body weight of lidocaine HCI (2.5)
—- DOSAGE FORMS AND STRENGTHS —-
- 120 mg per 6 mL Prefilled Syringe (3)
- 220 mg per Tl mL Prefilled Syringe (3)
——— CONTRAINDICATIONS ———
- Known hypersensitivity to any local anesthetic agent of the amide-type or to other components of GLYDO 2% Jelly (4.1)
- Infected and/or Severely Traumatized Mucosa (4.2)
- Severe shock or heart block (4.3)
—– WARNINGS AND PRECAUTIONS —–
- Dose-Related Toxicity: follow dosing instructions carefully. (5.1)
- Methemoglobinemia: Cases have been reported in association with local anesthetics use. See full prescribing information for more details on managing these risks. (5.2)
- Familial Malignant Hyperthermia: Monitoring of patients is recommended (5.3)
- Endotracheal Tube Occlusion: Avoid introduction of jelly into the lumen of the endotracheal tube (5.4)
- Risk of Aspiration and Biting Trauma with Oral Use: Food and chewing gum should not be taken while the mouth or throat area is anesthetized (5.7)
——— ADVERSE REACTIONS ———
Most common adverse reactions are as follows:
Central Nervous System: Lightheadedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. (6)
Cardiovascular System: Bradycardia, hypotension, and cardiovascular collapse. (6)
Allergic: Cutaneous lesions, urticaria, edema or anaphylactoid reactions. (6)
Neurologic: Positional hypotension and backache. (6)
Hematologic: Methemoglobinemia. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Sagent Pharmaceuticals at 1-866-625-1618 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
———DRUG INTERACTIONS ———
Local Anesthetics: The toxic effects of local anesthetics are additive. Monitor for neurologic and cardiovascular effects when additional local anesthetics are administered (7.1).
Drugs Associated with Methemoglobinemia: Patients are at increased risk of developing methemoglobinemia when concurrently exposed to nitrates, nitrites, local anesthetics, antineoplastic agents, antibiotics, antimalarials, anticonvulsants, and other drugs (7.2).
Hepatic Impairment: Consider reduced dosing and increased monitoring for local anesthetic systemic toxicity in patients with hepatic impairment (8.6)
—– USE IN SPECIFIC POPULATIONS —–
Pediatric Use: Dose should be reduced commensurate with age, body weight and physical condition (8.4)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 05/2025
______________________________________________________________________________________________________________
FULL PRESCRIBING INFORMATION: CONTENTS*
- INDICATIONS AND USAGE
- DOSAGE AND ADMINISTRATION
2.1 For Surface Anesthesia of the Male Adult Urethra
2.2 For Surface Anesthesia of the Female Adult Urethra
2.3 Lubrication for Endotracheal Intubation
2.4 Dosing for Pediatric Patients
2.5 Administration Instructions - DOSAGE FORMS AND STRENGTHS
- CONTRAINDICATIONS
4.1 Hypersensitivity
4.2 Use on Infected and/or Severely Traumatized Mucosa
4.3 Use in Severe Shock or Heart Block - WARNINGS AND PRECAUTIONS
5.1 Dose Related Toxicity
5.2 Methemoglobinemia
5.3 Familial Malignant Hyperthermia
5.4 Endotracheal Tube Occlusion
5.5 Anaphylactic Reactions
5.6 Risk of Toxicity in Patients with Hepatic Impairment
5.7 Risk of Aspiration and Biting Trauma with Oral Use - ADVERSE REACTIONS
- DRUG INTERACTIONS
7.1 Local Anesthetics
7.2 Drugs Associated with Methemoglobinemia - USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
10. OVERDOSAGE
11. DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
17.1 Allergic Type Reactions
17.2 Methemoglobinemia
17.3 Aspiration
17.4 Risk of Biting Trauma
* Sections or subsections omitted from the full prescribing information are not listed.
_____________________________________________________________________________________________________________
FULL PRESCRIBING INFORMATION
1. INDICATIONS AND USAGE
GLYDO (lidocaine HCl jelly) 2% is an amide local anesthetic indicated:
- for prevention and control of pain in procedures involving the male and female urethra
- for topical treatment of painful urethritis
- as an anesthetic lubricant for oral and nasal endotracheal intubation
2. DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Information
Administration Precautions
The toxic effects of local anesthetics are additive. Monitor for neurologic and cardio-vascular effects related to local anesthetic systemic toxicity when additional local anesthetics are administered with GLYDO (lidocaine HCI jelly) 2% [see Warnings and Precautions (5.1), Adverse Reactions (6), Overdosage (i0}].
The dosage varies and depends upon the area to be anesthetized, vascularity of the tissues, individual tolerance, and the technique of anesthesia. The lowest dosage needed to provide effective anesthesia should be administered. Dosages should be reduced for children and for elderly and debilitated patients.
Although the incidence of adverse effects with GLYDO (lidocaine HCl jelly) 2% is quite low, caution should be exercised, particularly when employing large amounts, since the incidence of adverse effects is directly proportional to the total dose of local anesthetic agent administered.
No more than 600 mg of lidocaine HCI should be given in any 12 hour period.
2.2 For Surface Anesthesia of the Male Adult Urethra
Slowly instill approximately 15 mL (300 mg of lidocaine HCl) into the urethra. Apply a penile clamp for several minutes at the corona. An additional dose of not more than 15 mL (300 mg} can be instilled if needed.
Prior to sounding or cystoscopy, a penile clamp should be applied for S to 10 minutes to obtain adequate anesthesia. A total dose of 30 mL (600 mg) is usually required to fill and dilate the male urethra.
Prior to catheterization, 5 mL to 10 mL (100 mg to 200 mg) are recommended for lubrication.
2.3 For Surface Anesthesia of the Female Adult Urethra
Slowly instill approximately 3 mL to 5 mL (60 mg to 100 mg of lidocaine HCl) into the urethra. In order to obtain adequate anesthesia, wait for several minutes prior to performing urological procedures. If desired, some jelly may be deposited on a cotton swab and introduced into the urethra.
2.4 Lubrication for Endotracheal Intubation
Apply a sufficient amount of jelly to coat the external surface of the endotracheal tube shortly before use. Care should be taken to avoid introducing the product into the lumen of the tube.
Do not use the jelly to lubricate endotracheal stylettes. (see WARNINGS and ADVERSE REACTIONS concerning rare reports of inner lumen occlusion). It is also recommended that use of endotracheal tubes with dried jelly on the external surface be avoided for lack of lubricating effect.
2.5 Dosing for Pediatric Patients
Amaximum dose of GLYDO (lidocaine HCl jelly) 2% for children varies based on age and weight. The maximum dose should not exceed 4.5 mg/ kg of body weight. For children over 3 years of age, the maximum dose is determined by the child’s age and weight. For example, in a child of 5 years weighing approximately 23 kg, the dose of lidocaine hydrochloride should not exceed approximately 75 mg to 100 mg (3.3 mg/ kg to 4.4 mg/kg).
The lowest effective dose should be used
3. DOSAGE FORMS AND STRENGTHS GLYDO (lidocaine HCl jelly, USP) 2% in:
- 120 mg per 6 mL Prefilled Syringe
- 220 mg per Tl mL Prefilled Syringe
4. CONTRAINDICATIONS
4.1 Hypersensitivity
GLYDO 2% Jelly is contraindicated in patients with a known history of hypersensitivity to lidocaine or to any local anesthetics of the amide type or to other components of GLYDO 2% Jelly.
4.2 Use on Infected and/or Severely Traumatized Mucosa
GLYDO 2% Jelly should not be used on infected and/or severely traumatized mucosa in the area of application.
4.3 Use in Severe Shock or Heart Block
GLYDO 2% Jelly should not be used in patients with severe shock or heart block.
5. WARNINGS AND PRECAUTIONS
5.1 Dose-Related Toxicity
The safety and effectiveness of GLYDO 2% Jelly depends on proper dosage, correct technique, adequate precautions, and readiness for emergencies [see Adverse Reactions (6)]. Careful and constant monitoring of cardiovascular and respiratory (adequacy of ventilation) vital signs and the patient’s state of consciousness should be performed after application of GLYDO 2% Jelly. Possible early warning signs of central nervous system (CNS) toxicity are restlessness, anxiety, incoherent speech, lightheadedness, numbness and tingling of the mouth and lips, metallic taste, tinnitus, dizziness, blurred vision, tremors, twitching, CNS depression, or drowsiness. Delay in proper management of dose-related toxicity, underventilation from any cause, and/or altered sensitivity may lead to the development of acidosis, cardiac arrest, and, possibly, death.
Use the lowest dosage that results in effective anesthesia to avoid high plasma levels and serious adverse effects. Repeated doses of lidocaine may cause significant increases in blood levels with each repeated dose because of slow accumulation of the drug or its metabolites. Tolerance to elevated blood levels varies with the status of the patient. Debilitated, elderly patients, acutely ill patients, and children should be given reduced doses commensurate with their age and physical status.
Patients and healthcare providers should be instructed to strictly adhere to the recommended dosage and administration guidelines as set forth in this package insert. The management of serious adverse reactions may require the use of resuscitative equipment, oxygen, and other resuscitative drugs.
5.2 Methemoglobinemia
Cases of methemoglobinemia have been reported in association with local anesthetic use. Although all patients are at risk for methemoglobinemia, patients with glucose-6-phosphate dehydrogenase deficiency, congenital or idiopathic methemoglobinemia, cardiac or pulmonary compromise, infants
under 6 months of age, and concurrent exposure to oxidizing agents or their metabolites are more susceptible to developing clinical manifestations of the condition [see Drug Interactions (7.2)]. If local
anesthetics must be used in these patients, close monitoring for symptoms and signs of methemoglobinemia is recommended.
Signs of methemoglobinemia may occur immediately or may be delayed some hours after exposure, and are characterized by a cyanotic skin discoloration and/or abnormal coloration of the blood. Methemoglobin levels may continue to rise; therefore, immediate treatment is required to avert more serious central nervous system and cardiovascular adverse effects, including seizures, coma, arrhythmias, and death. Discontinue GLYDO 2% Jelly and any other oxidizing agents. Depending on the severity of the signs and symptoms, patients may respond to supportive care, i.e., oxygen therapy, hydration. A more severe clinical presentation may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
5.3 Familial Malignant Hyperthermia
Many drugs used during the conduct of anesthesia are considered potential triggering agents for familial malignant hyperthermia. Since it is not known whether amide-type local anesthetics may trigger this reaction and since the need for supplemental general anesthesia cannot be predicted in advance, it is suggested that a standard protocol for management should be available. Early unexplained signs of tachycardia, tachypnea, labile bloodpressure, and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, promptdiscontinuance of the suspect triggering agent(s) and institution of treatment, including oxygen therapy, indicated supportive measuresand dantrolene (consult dantrolene sodium intravenous package insert before using).
5.4 Endotracheal Tube Occlusion
When used for endotracheal tube lubrication, care should be taken to avoid introducing the product into the lumen of the tube. Do not use the jelly to lubricate the endotracheal stylettes. If allowed into the inner lumen, the jelly may dry on the inner surface leaving a residue which tends to clump with flexion, narrowing the lumen. There have been rare reports in which this residue has caused the lumen to occlude [see Adverse Reactions (6) and Dosage and Administration (2)].
5.5 Anaphylactic Reactions
Anaphylactic reactions may occur following administration of lidocaine hydrochloride [see Adverse Reactions (6)]. Patients allergic to para-aminobenzoic acid derivatives (procaine, tetracaine, benzocaine, etc.) have not shown cross sensitivity to lidocaine.
5.6 Risk of Toxicity in Patients with Hepatic Impairment
Because amide local anesthetics such as lidocaine are metabolized by the liver, consider reduced dosing and increased monitoring for lidocaine systemic toxicity in patients with moderate to severe hepatic impairment who are treated with GLYDO 2% Jelly, especially with repeat doses [see Use in Specific Populations (8.6)].
5.7 Risk of Aspiration and Biting Trauma with Oral Use
When used orally (i.e. endotracheal tube lubrication), topical anesthesia may occur to oropharyngeal structures. This may impair swallowing and thus enhance the danger of aspiration. For this reason, food should not be ingested for 60 minutes following use of local anesthetic preparations in the mouth or throat area. This is particularly important in children because of their frequency of eating.
Numbness of the tongue or buccal mucosa may enhance the danger of unintentional biting trauma. Food and chewing gum should not be taken while the mouth or throat area is anesthetized.
6. ADVERSE REACTIONS
The following adverse reactions associated with the use of GLYDO 2% Jelly were identified in clinical studies or postmarketing reports. Because some of these reactions were reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Adverse experiences following the administration of lidocaine are similar in nature to those observed with other amide local anesthetic agents. A major cause of adverse reactions to this group of drugs is excessive plasma levels, which may be due to overdosage or slow metabolic degradation.
The most commonly encountered acute adverse reactions that demand immediate counter measures were related to the CNS and the cardiovascular system. These adverse experiences are, in general, dose-related and may result from high plasma levels caused by excessive dosage or rapid absorption, or may result from a hypersensitivity, idiosyncrasy, or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported.
There have been rare reports of endotracheal tube occlusion associated with the presence of dried jelly residue in the inner lumen of the tube.
Nervous System Disorders
Adverse reactions were characterized by excitation and/or depression of the central nervous system and included lightheadedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression, and arrest. The excitatory manifestations may be very brief or may not occur at all, in which case the first manifestation of toxicity may be drowsiness merging into unconsciousness and respiratory arrest.
Drowsiness following the administration of lidocaine is usually an early sign of a high blood level of the drug and may occur as a consequence of rapid absorption.
Cardiac Disorders
High doses have led to high plasma levels and related depression of the myocardium, decreased cardiac output, heartblock, hypotension, bradycardia, and cardiovascular collapse, which may lead to cardiac arrest.
Immune System Disorders
Allergic reactions are characterized by cutaneous lesions, urticaria, edema, or anaphylactoid reactions. Allergic reactions may occur as a result of sensitivity either to the local anesthetic agent or to other components in the formulation.
7. DRUG INTERACTIONS
7.1 Local Anesthetics
The toxic effects of local anesthetics are additive. If coadministration of other local anesthetics with GLYDO 2% Jelly cannot be avoided, monitor patients for neurologic and cardiovascular effects related to local anesthetic systemic toxicity [see Warnings and Precautions (5.1)].
7.2 Drugs Associated with Methemoglobinemia
Patients who are administered local anesthetics are at increased risk of developing methemoglobinemia when concurrently exposed to the following drugs, which could include other local anesthetics:
Examples of Drugs Associated with Methemoglobinemia:
| Class | Examples |
| Nitrates/Nitrites | nitric oxide, nitroglycerin, nitroprusside, nitrous oxide |
| Local anesthetics | articaine, benzocaine, bupivacaine, lidocaine, mepivacaine, prilocaine, procaine, ropivacaine, tetracaine |
| Antineoplastic Agents | cyclophosphamide, flutamide, hydroxyurea, ifosfamide, rasburicase |
| Antibiotics | dapsone, nitrofurantoin, para-aminosalicylic acid, sulfonamides |
| Antimalarials | chloroquine, primaquine |
| Anticonvulsants | Phenobarbital, phenytoin, sodium valproate |
| Other drugs | acetaminophen, metoclopramide, quinine, sulfasalazine |
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available published data and decades of clinical use with GLYDO 2% Jelly in pregnant women have not identified any drug-associated riskcfor major birth defects, miscarriage, or other adverse maternal or fetal outcomes. Local anesthetics may cause varying degrees of toxicity to the mother and fetus and adverse reactions include alterations of the centralnervous system, peripheral vascular tone and cardiac function {see Clinical Considerations].
There was no evidence of teratogenicity when lidocaine was administered to pregnant rats and rabbits subcutaneously at 0.8 and 0.16 times, respectively, the maximum recommended human dose (MRHD) of 600 mg during the period of organogenesis. In a published animal reproduction study, pregnant rats administered lidocaine by continuous subcutaneous infusion at 8 times the MRHD during the period of organogenesis resulted in lower fetal body weights [see Data].
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risks of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Maternal adverse reactions
During treatment of systemic toxicity, which may appear as maternal hypotension or fetal bradycardia, the parturient should be maintained in the left lateral decubitus position if possible or manual displacement of the uterus off the great vessels be accomplished. Elevating the patient’s legs will also help prevent decreases in blood pressure. The fetal heart rate also should be monitored continuously, and electronic fetal monitoring is highly advisable.
Labor or delivery
Local anesthetics rapidly cross the placenta and can cause varying degrees of maternal, fetal and neonatal toxicity {see Clinical Pharmacology (12.3)]. The incidence and degree of toxicity depend upon the procedure performed, the type and amount of drug used, and the technique of drug administration. Adverse reactions in the parturient, fetus and neonate involve alterations of the central nervoussystem, peripheral vascular tone, and cardiac function. However, dosage recommendations for local anesthesia are much lower than dosage recommendations for other major blocks.
Data
Animal Data
Reproduction studies for lidocaine have been performed in both rats and rabbits. There was no evidence of harm to the fetus when pregnant rats were given subcutaneous doses of up to 50 mg/kg lidocaine (approximately 0.8 times the MRHD of 600 mg based on body surface area (BSA) comparison) during the period of organogenesis. In addition, there was no evidence of harm to the fetus when pregnant rabbits were given a subcutaneous dose of 5 mg/kg (approximately 0.16 times the MRHD based on BSA comparison) during the period of organogenesis. Treatment of pregnant rabbits with 25 mg/kg (approximately 0.8 times the MRHD based on BSA comparison) produced evidence of maternal toxicity and evidence of delayed fetal development, including a non- significant decrease in fetal weight (7%) and an increase in minor skeletal anomalies (skull and sternebral defect, reduced ossification of the phalanges).
The effect of lidocaine on _ post-natal development was examined in rats by treating pregnant female rats daily subcutaneously at doses of 2, 10, and 50 mg/kg (approximately 0.03, 0.16, and 0.8 times, respectively, the MRHD based on BSA comparison) from Day 15 of pregnancy and up to 20 days postpartum. No signs of adverse effects were seen either in dams or in the pups up to and including the dose of 10 mg/kg; however, the number of surviving pups was reduced at 50 mg/kg, both at birth and the duration of lactation period, the effect most likely being secondary to maternal toxicity. No other effects on litter size, litter weight, abnormalities in the pups and physical developments of the pups were seen in this study.
A second study examined the effects of lidocaine on post-natal development in the rat that included assessment of the pups from weaning to sexual maturity. Rats were treated for 8 months with 10 or 30 mg/kg, s.c. lidocaine (approximately 0.8 and 1.6 times, respectively, the MRHD based on BSA comparison). This time period encompassed 3 mating periods. There was no evidence of altered post-natal development in any offspring; however, both doses of lidocaine significantly reduced the average number of pups per litter surviving until weaning of offspring from the first 2 mating periods.
In a published study, lidocaine administered to pregnant rats by continuous subcutaneous infusion during the period of organogenesis at 100, 250, and 500 mg/kg/day, did not produce any structural abnormalities, but did result in lower fetal weights at 500 mg/kg/day dose (approximately 8 times the MRHD based on BSA comparison) in the absence of maternal toxicity.
8.2 Lactation
Risk Summary
Published data report the presence of lidocaine and its metabolites in human milk in low amounts, along with poor oral bioavailability. There are no data on the effect of lidocaine on the breastfed infant or the effect on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for GLYDO 2% Jelly and any potential adverse effects on the breastfed child from GLYDO 2% Jelly or from the underlying maternal condition.
8.4 Pediatric Use
Although the safety and effectiveness of GLYDO 2% Jelly in pediatric patients have not been established, a study of 19 premature neonates (gestational age <33 weeks) found nocorrelation between the plasma concentration of lidocaine
or monoethylglycinexylidide and infant body weight when moderate amounts of lidocaine (ie. 0.3 mL/kg of lidocaine gel 20 mg/mL) were used for lubricating both intranasal and endotracheal tubes. No neonate had plasma
levels of lidocaine above 750 mcg/L. Dosages in children should be reduced, commensurate with age, body weight, and physical condition [see Dosage and Administration (2)].
8.5 Geriatric Use
Elderly patients should be given reduced doses commensurate with their age and physical condition.
8.6 Hepatic Impairment
Amide-type local anesthetics such as lidocaine are metabolized by the liver. Patients with severe hepatic impairment, because of their inability to metabolize local anesthetics normally, are at greater risk of developing toxic plasma
concentrations and potentially local anesthetic systemic toxicity. Therefore, consider reduced dosing and increased monitoring for local anesthetic systemic toxicity in patients with hepatic impairment treated with GLYDO 2% Jelly especially with repeat doses [see Warnings and Precautions (5.6)].
10. OVERDOSAGE
Acute emergencies from local anesthetics are generally related to high plasma levels encountered during therapeutic use of local anesthetics [see Warnings and Precautions (5) and Adverse Reactions (6)]. Tne use of this product concomitantly with other lidocaine products should be done with caution and appropriate patient monitoring.
Management of Local Anesthetic Emergencies
The first consideration is prevention, best accomplished by careful and constant monitoring of cardiovascular and respiratory vital signs and the patient’s state of consciousness after each local anesthetic administration. At the first sign of change, oxygen should be administered.
The first step in the management of convulsions consists of immediate attention to the maintenance of a patent airway and assisted or controlled ventilation with oxygen and a delivery system capable of permitting immediate positive airway pressure by mask. Immediately after the institution of these ventilatory measures, the adequacy of the circulation should be evaluated, keeping in mind that drugs used to treat convulsions sometimes depress the circulation when
administered intravenously. Should convulsions persist despite adequate respiratory support, and if the status of the circulation permits, a benzodiazepine (such as diazepam) may be administered intravenously. The clinician should be familiar, prior to use of local anesthetics, with these anticonvulsant drugs. Supportive treatment of circulatory depression may require administration of intravenous fluids and, when appropriate, a vasopressor as directed by the clinical situation (e.g., ephedrine).
If not treated immediately, both convulsions and cardiovascular depression can result in hypoxia, acidosis, bradycardia, arrhythmias, and cardiac arrest. If cardiac arrest should occur, standard cardiopulmonary resuscitative measures should be instituted.
Endotracheal intubation, employing drugs and techniques familiar to the clinician, may be indicated, after initial administration of oxygen by mask; if difficulty is encountered in the maintenance of a patient airway or if prolonged ventilatory support (assisted or controlled) is indicated.
Dialysis is of negligible value in the treatment of acute overdosage with lidocaine.
11. DESCRIPTION
GLYDO (lidocaine HCl jelly, USP) 2% is a sterile aqueous product that contains a local anesthetic agent and is administered topically (see INDICATIONS AND USAGE for specific uses).
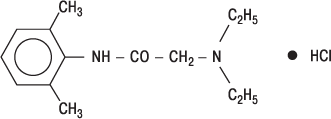
GLYDO (lidocaine HCI jelly, USP) 2% contains lidocaine HCl which is chemically designated as acetamide, 2-(diethylamino)- N-(2,6-dimethylphenyl)-, | monohydrochloride, the molecular weight is 270.8. The molecular formula is C14H23CIN2O, and has the following structural formula:
GLYDO (lidocaine HCl jelly, USP) 2% also contains hypromellose, and the resulting mixture maximizes contact with mucosa and provides lubrication for instrumentation. The unused portion should be discarded after initial use,
Composition of GLYDO (lidocaine HCl jelly, USP) 2% 6 mL or Tl mL syringes: Each mL contains 20 mg of lidocaine HCI. The formulation also contains hypromellose, and sodium hydroxide to adjust pH to 6.0 to
7.0.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Lidocaine stabilizes the neuronal membrane by inhibiting the ionic fluxes required for the initiation and conduction of impulses, thereby effecting local anesthetic action.
12.2 Pharmacodynamics
The onset of action is 3 to 5 minutes. It is ineffective when applied to intact skin.
Excessive blood levels may cause changes in cardiac output, total peripheral resistance, and mean arterial pressure. These changes may be attributable to a direct depressant effect of the local anesthetic agent on various components of the cardiovascular system.
Factors such as acidosis and the use of CNS stimulants and depressants affect the CNS levels of lidocaine hydrochloride required to produce overt systemic effects. Objective adverse manifestations become increasingly apparent with increasing venous plasma levels above 6 mcg free base per mL. In the rhesus monkey arterial blood levels of 18 to 21 meg/mL have been shown to be threshold for convulsive activity.
12.3 Pharmacokinetics
Absorption
Lidocaine may be absorbed following topical administration to mucous membranes, its rate and extent of absorption depending upon concentration and total dose administered, the specific site of application, and duration of exposure. In general, the rate of absorption of local anesthetic agents following topical application occurs most rapidly after intratracheal administration. Lidocaine is also well-absorbed from the gastrointestinal tract, but little intact drug may appear in the circulation because of biotransformation in the liver.
Distribution
The plasma binding of lidocaine is dependent on drug concentration, and the fraction bound decreases with increasing concentration. At concentrations of 1to 4 mcg of free base per mL, 60 to 80 percent of lidocaine is protein bound. Binding is also dependent on the plasma concentration of the alpha-l-acid glycoprotein. Lidocaine crosses the blood-brain and placental barriers, presumably by passive diffusion.
Elimination
Lidocaine is metabolized rapidly by the liver, and metabolites and unchanged drug are excreted by the kidneys. Biotransformation includes oxidative N-dealkylation, ring hydroxylation, cleavage of the amide linkage, and conjugation. N-dealkylation, a major pathway of biotransformation, yields the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological actions of these metabolites are similar to, but less potent than, those of lidocaine. Approximately 90% of lidocaine administered is excreted in the form of various metabolites, and less than 10% is excreted unchanged.
The primary metabolite in urine is a conjugate of 4-hydroxy-2,6-dimethylaniline.
Studies of lidocaine metabolism following intravenous bolus injections have shown that the elimination half-life of this agent is typically 15 to 2 hours, Because of the rapid rate at which lidocaine is metabolized, any condition that affects liver function may alter lidocaine kinetics. The half-life may be prolonged twofold or more in patients with liver dysfunction. Renal dysfunction does not affect lidocaine kinetics but may increase the accumulation of metabolites.
13. NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term studies in animals have not been performed to evaluate the carcinogenic potential of lidocaine.
Mutagenesis
The mutagenic potential of lidocaine has been tested in the Ames Salmonella reverse mutation assay, an in vitro chromosome aberrations assay in human lymphocytes and in an in vivo mouse micronucleus assay. There was no indication of any mutagenic effect in these studies.
Impairment of Fertility
The effect of lidocaine on fertility was examined in the rat model. Administration of 30 mg/kg, s.c. (approximately 0.5 times the MRHD based on BSA comparison) to the mating pair did not produce alterations in fertility or general reproductive performance of rats. There are no studies that examine the effect of lidocaine on sperm parameters. There was no evidence of altered fertility.
In a published study, female Sprague-Dawley rats were treated subcutaneously with lidocaine via osmotic pumps starting two weeks prior to mating, and reproductive effects were assessed. Rats dosed up to 250 mg/kg/ day (approximately 4 times the MRHD based on BSA comparison) showed no effects on copulatory rate, pregnancy rate, numbers of corpora lutea, or implantations.
16. HOW SUPPLIED/STORAGE AND HANDLING
GLYDO? (lidocaine HCl jelly, USP) 2% is supplied as follows:
| GLYDO® (lidocaine HCl jelly, USP) 2% | ||
| NDC | (20 mg per mL) | Package factor |
| 25021-673-76 | 120 mg per 6 mL Single-Dose Prefilled Syringe | 10 syringes per carton |
| 25021-673-77 | 220 mg per 11 mL Single-Dose Prefilled Syringe | 10 syringes per carton |
Storage Conditions
Store at 20° to 25°C (68° to 77°F} [See USP
Controlled Room Temperature].
Discard unused portion.
Sterile, Preservative-free, PVC-free. The container and container closure are not made with natural rubber latex.
17. PATIENT COUNSELING INFORMATION
17.1 Allergic-Type Reactions
Assess if the patient has had allergic-type reactions to amide-type local anestheticsor to other formulation ingredients [see Contraindications (4), Warnings and Precautions (5.6), Adverse Reactions (6)].
17.2 Methemoglobinemia
Inform patients that use of local anesthetics may cause methemoglobinemia, a serious condition that must be treated promptly.
Advise patients or caregivers to stop use and seek immediate medical attention if they or someone in their care experience the following signs or symptoms: pale, gray, or blue colored skin (cyanosis); headache; rapid heart rate; shortness of breath; lightheadedness; or fatigue [see Warnings and Precautions (5.2)].
17.3 Risk of Aspiration
When topical anesthetics are used in the mouth, the patient should be aware that the production of topical anesthesia may impair swallowing and thus enhance the danger of aspiration. For this reason, food should not be ingested for 60 minutes following use of local anesthetic preparations in the mouth or throat area. This is particularly important in children because of their frequency of eating.
17.4 Risk of Biting Trauma
Numbness of the tongue or buccal mucosa may enhance the danger of unintentional biting trauma. Food and chewing gum should not be taken while the mouth or throat area is anesthetized.
Brands listed are the trademarks of their respective owners.
INSTRUCTIONS FOR USE
Please note: The blister package contains a sterile syringe.
Do not open the blister until ready to use.
- When ready to use, open the blister and drop the syringe onto a sterile field.
- Before removing the tip cap, press in the plunger to remove any resistance that may be present. This helps ensure that the syringe will empty easily and uniformly.
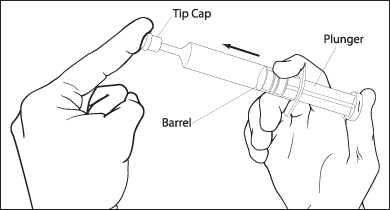
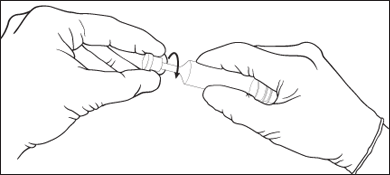
- Remove the tip cap from the syringe. The syringe is now ready for use.
- GLYDO (lidocaine HCl jelly, USP) 2% should be instilled slowly and evenly into the urethra. See the DOSAGE AND ADMINISTRATION section for additional details.
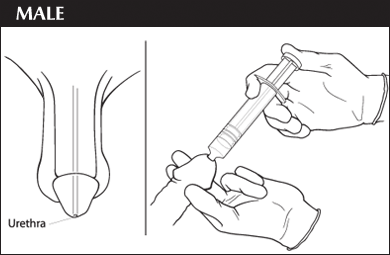
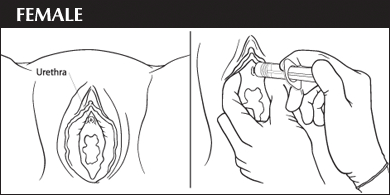
- Wait for a few minutes after instillation of GLYDO (lidocaine HCl jelly, USP) 2% for the anesthetic to take full effect. Full anesthetic effect will occur in 5 to 10 minutes after complete instillation.
- Any gel not used in a single application must be discarded.
Mfd. for SAGENT Pharmaceuticals
Schaumburg, IL 60173 (USA)
Mfd. by Klosterfrau Berlin GmbH
Made in Germany
©2025 Sagent Pharmaceuticals
Revised: May 2025
This “Instructions for Use” has been approved by the U.S. Food and Drug Administration.

